During some of your sessions, and while we were trying to explain what we’ve found or what we think was happening in your body, you may have heard us using terms like “intraosseous” tensions, or tensions “inside the bone itself”. I get how it can sound a bit weird or how such a concept may seem strange at first, so what I propose to do today is to try and explain it in more detail, learn more about your bones and how this can affect your body.
Getting intimate with your bones
First thing to do is to get to know your bones a bit better…what they really are, their purpose and what they’re made of. Once you know their structures and functions, then we can start to see how they work.
Functions
Our bones are under-estimated. Obviously without them we would be way less sexy, looking more like a sort of big slug crawling on the ground, but there’s a lot more about them than that…they fulfill no less than 7 functions for your body.
Support – the bones make a rigid structure which acts like a support for our body and our soft organs.
Protection – your brain is well-sheltered inside your skull, your vertebrae wrap your spinal cord and your rib cage protects your vital organs.
Anchor – your muscles are fixated to your bones and use them as levers to allow movements, actions, breathing.
Storage of minerals – bones are an important storage for minerals especially calcium and phosphor which can be liberated into the blood when needed.
Formation of blood cells – in adults, the formation of blood cells happens in the “red” bone marrow of some bones.
Storage of Lipids – Lipids are stocked as “yellow” bone marrow in long bones, it’s a reserve of energy for your organism.
Production of hormones – bones are producing osteocalcin, a hormone which contributes to the regulation of the secretion of insulin, to the homeostasis of the glucose and to the energy expenditure.
Anatomy
We could spend hours talking about bone anatomy if we would go in all the details, but that’s not the point here so we’ll keep it simple, just enough to understand what’s coming next.
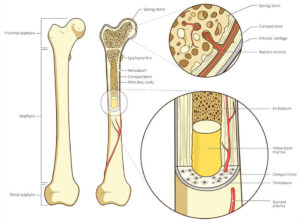 Each bone is composed by an external layer very dense, the cortical bone (or compact bone), in which there is an internal layer, constituted by small cavities, spans, and bone trabeculae, the cancellous bone (or spongy bone). These cavities contain the bone marrow.
Each bone is composed by an external layer very dense, the cortical bone (or compact bone), in which there is an internal layer, constituted by small cavities, spans, and bone trabeculae, the cancellous bone (or spongy bone). These cavities contain the bone marrow.
There is 2 kinds of bones, the short bones (flat, like the bones of your skull or the sternum) and long bones (like the femur in your leg or the humerus in your arm). The long bones also have a big and central cavity in the middle, the medullary cavity, filled by “yellow” bone marrow (storage for lipids), whereas the “red” bone marrow (responsible for the formation of blood cells) is located in the cancellous bone in the extremities of long bones or in short bones.
Extremities are covered by cartilage where there is a joint with an other bone, while the rest of the bone is wrapped in a membrane with a lot of nerves, vascular elements, and osteogenic cells (involved in the bone remodeling), the periosteum.
Cells
There are 5 main kind of cells in the bone tissue:
Osteogenic (or Osteoprogenitor) cells which are stem cells who will be able to become osteoblasts or parietal cells when stimulated.
Osteoblasts which produce bone tissue.
Osteocytes which regulate and maintain the bone matrix, and also act as tension detectors and react to mechanical stimulus like weight, deformation…
Parietal cells, at the surface of the bone when no remodeling is happening.
Osteoclasts which degrade bone tissue.
Chemical composition
The bone contains both organic (cells, proteins, fibers, bone ground substance) and non-organic (minerals) components. It’s the right combination which makes the bone extremely durable and resistant without becoming breakable (to a certain point of course).
When you compare the bone with steel, a healthy bone is half less resistant to pressure but is as resistant to tension.
It’s alive!
As any tissue in your body, the bone tissue was created while you were an embryo, and then kept growing and aging with you. It’s always changing and adapting to its environment, to the forces applied to it, remodeling itself to always be as efficient as possible in its roles. So yes, it’s definitely a living tissue!
Before the 8th week of gestation, the skeleton of the human embryo is entirely constituted by membranes and cartilages. Then, the bone tissue will progressively replace most of these structures.
Bones will keep growing in length and diameter until you become a young adult where most of them stop growing except some bone of the face like the nose and the jaw which will keep growing but almost unperceptively all your life.
But that doesn’t mean your bones are dead. In fact, there will be permanent movements, changes happening in them, some bone tissue will be degraded while some other will be produced, to adapt, it’s called the bone remodeling.
In children and teenagers, there is more production than degradation of the bone tissue. In young adults, these 2 processes are balanced while the more you’re aging and the more the degradation is becoming predominant.
Bone remodeling
The bone tissue is very active and dynamic, and small changes in its architecture are continuously happening. Every year, 5 to 10% of our skeleton is being replaced which means our whole skeleton is replaced every 10 years (don’t get me wrong, it doesn’t mean you get brand new bones every 10 years, as nice as it would be, it doesn’t work that way, it’s a progressive process happening bit by bit over 10 years).
The degradation of the bone tissue is executed by the osteoclasts which will secrete acid to dissolve the bone matrix and the minerals like Calcium for instance, and then release them in the blood.
The new bone tissue is created by the osteoblasts which will bring some new bone matrix which contains specific proteins which will fix the calcium.
Of course we simplified it because it’s a bit more complicated than that 🙂
Regulation
This remodeling which is constantly happening in our skeleton is under the influence of 2 “loops” of regulation with different functions.
Hormonal regulation – its purpose is to maintain the homeostasis of the calcium in the blood.
 Just to clarify for those who don’t know what homeostasis is: it’s the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and includes many variables being kept within certain pre-set limits (homeostatic range).
Just to clarify for those who don’t know what homeostasis is: it’s the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and includes many variables being kept within certain pre-set limits (homeostatic range).
So in our case, if the concentration of calcium in the blood falls under its normal values, it stimulates the parathyroid glands which will secrete parathormone (or parathyroid hormone, PTH) which in turn will activate the osteoclasts to degrade bone tissue and release calcium in the blood.
Put it simply, this regulation determines if and when a remodeling is needed.
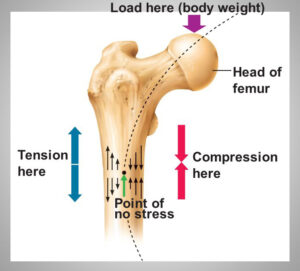 Mechanical regulation – it’s the reaction to mechanical solicitations (muscles traction) and gravitational force. It aims at reinforcing the bone where it endures strong constraints. Thus the thickness of a same and one bone won’t be equal all along itself, and the trabeculae of the cancellous bone will form a mesh which follows the lines of compression for instance.
Mechanical regulation – it’s the reaction to mechanical solicitations (muscles traction) and gravitational force. It aims at reinforcing the bone where it endures strong constraints. Thus the thickness of a same and one bone won’t be equal all along itself, and the trabeculae of the cancellous bone will form a mesh which follows the lines of compression for instance.
Fun fact, because they’re not affected by the gravitational force, astronauts lose 0.5% of their bone mass by month spent in space.
If the hormonal regulation was determining if and when a remodeling would happen, the mechanical regulation would determine where depending on the different forces and constraints applied to the bones.
Why it is interesting (… or at least your Osteopathic Practitioner thinks so 🙂 )
When there is a trauma, strong forces can be applied to your bones. For instance, in a car accident there will be the inertia of the movement, the shock of the contact, the strength of the seat belt trying to hold you…all of this could be pretty strong and violent on your bones – well, on your whole body to be honest but here we’re focusing on bones. Such violent forces could result in slight changes in the lines of compression in the architecture of your bones. Slight but enough to have consequences like the modifications of the surrounding soft tissues which will adapt to the new distribution of the forces, changing the way the tensions are distributed.
If we don’t address these intraosseous tensions and torsions, then they will keep impacting in the rest of the body in different ways.
That’s how a shoulder could still be restricted and painful and/or weak long after a car accident…the seat belt may have applied a strong force on your clavicle. That’s how you might still not trust an ankle long after a sprain or even feel like your bone is painful right above the malleoli where the Fibula had to endure torsion on itself. That’s why it’s interesting for your Osteopathic Practitioner to address these tensions too because they can be part of the dysfunctional scheme your body is compensating for.
As an extra note, even though it’s frequent during violent traumas, it doesn’t require one to create intraosseous tensions. The same force applied repeatedly every day doesn’t have to be strong to make the lines of compression change as the bone is remodeled depending on the forces applied to it. Let’s say you have to put yourself in a specific prolonged posture every day for work, the gravitational force will not be distributed the same way and your bones will adapt.
I hope this explained the concept of intraosseous tensions a little better and made it a bit more clear to you, but if you still have questions about it, feel free to contact us or leave a comment here.


Trackbacks/Pingbacks